The increase in life expectancy at birth witnessed in the twentieth century has been attributed to major public health achievements, including vaccination, control of infectious disease and reductions in tobacco use. Population aging came to be regarded as a triumph of modern life, with cancer, cardiovascular disease and dementia deemed to be the great obstacles to further progress in increasing health and life expectancy. The global pandemic of COVID-19 has brought infectious disease as a major threat to older persons back into sharp focus. The paper proposes five major changes to long-term care, with a view to protecting the elderly from the ravages of infectious disease while simultaneously providing greater quality of care and quality of life.
Introduction
The increase in life expectancy at birth witnessed in the twentieth century has been attributed to major public health achievements, including vaccination, control of infectious disease and reductions in tobacco use.1 In 1998, the secretary-general of the World Health Organization (WHO) stated, “We have another transition, the transition from the communicable to the non-communicable diseases.”2 She went on to state that attention to acute infectious disease and to chronic conditions “cannot be seen as competing tasks. They are complementary. We need to fight both.” By 2007, about three-quarters of all deaths in Canada and the United States occurred in people over 65. This value reached 80 percent in Canada in 2018.3 Population aging came to be regarded as a triumph of modern life, with cancer, cardiovascular disease and dementia deemed to be the great obstacles to further progress in increasing health and life expectancy. However, the global pandemic of COVID-19 has brought infectious disease as a major threat to older persons back into sharp focus.
By June 2020, the number of global COVID-19 cases approached 10 million individuals, with almost half a million deaths.5 The elderly are the most vulnerable to death due to the virus and account for the overwhelming majority of global COVID-19 deaths.6 While the pandemic has caused enormous social and economic upheaval in all sectors, it has proven to be particularly devastating for residents of long-term care (LTC) homes. In countries with more than 200 deaths per million population, the percentage of COVID-19 deaths occurring in LTC ranged from 15 percent in the Netherlands to 82 percent in Canada.7 When expressed as a rate per million population, the countries with the highest death toll in LTC by the end of May 2020 were Belgium (400), Spain (379), France (208), Ireland (184) and Italy (176).8 In terms of raw numbers, the United States stands out, with a minimal estimate of 40,600 nursing home deaths by early June 2020, or 450 residents per day since March.9 By the end of June, New York reported 6,427 LTC deaths, while in Massachusetts the toll was 5,007;10 in Canada, over the same time period, there were nearly 6,000 LTC home deaths.11 No matter how one quantifies the mortality experience in Europe and North America, it is fair to say that, unlike Severe Acute Respiratory Syndrome (SARS), COVID-19 has proven to be more of an LTC pandemic than one that affects the population at large.
With a few international exceptions, the initial response to COVID-19 in nursing homes was slow to develop. The narrow focus was on a potential crisis in hospitals. Regular elective procedures were postponed and an all-hands-on-deck approach was mounted for acute-care hospitals. However, with the passage of only one or two months, the devastation in LTC homes caused an outcry.12
Most healthy individuals do not want to end their lives in LTC. When asked about their preferences if they become unable to care for themselves for an extended period of time, only four percent of US survey respondents said they would want to move to a nursing home.13 Reports of horrible circumstances due to COVID-19 in some homes in Canada,14 Spain15 and the United States16 have exacerbated what were already stark impressions of these settings. At the same time, pictures emerged of heroic efforts by facilities, groups of facilities, and public authorities to hold off the early devastation.17 There is much to learn before we fully understand what transpired.
For some, an instinctive response has been to promote the elimination of LTC facilities altogether. It is argued that better community-based care would keep people in their homes at the end of their lives. As appealing as that idea is, it is unlikely to be feasible in those countries where there has been a major investment in LTC facilities. Home care also depends heavily on the willingness and ability of family members to provide about three-quarters of the care required by their loved ones.18 Changing family structures (e.g., divorce, childlessness), greater income disparities, dispersion of families due to increased geographic mobility, and changing labour force participation all portend a future where family members may be unable to provide 24/7 care in the community. Even in countries that have invested heavily in home-care services (Belgium, for example), the need remains for residential care for very frail older persons who do not have a cohabiting informal caregiver. Consequently, the need for congregate care settings will continue over time19 to support a population where gains in disability-free life expectancy are limited.
We may not eliminate the need for LTC homes, but there are compelling reasons to reimagine what those homes should be in the future.20 To that end, we propose five major areas of change for LTC.
1) Matching Clinical Resources to the Needs of LTC Residents
In most high-resource nations, nursing homes serve an increasingly medically complex and frail older population. Reports from the Centers for Disease Control (CDC), the WHO and the European Union from the outset of the COVID-19 pandemic identified older adults with underlying health conditions as being at highest risk of mortality.21 Based on those basic parameters, we analyzed assessment records from Canada, Finland, New Zealand and the United States to profile their nursing home residents and home care clients. Table 1 shows that the majority of persons in nursing home settings are 80 years of age or older (a similar pattern is evident in home care). Up to 90 percent of all residents have an underlying major comorbidity (such as heart failure, renal disease and neurological conditions). Indeed, about 60 percent of nursing home residents are aged 80 and over and have underlying comorbidities (not shown), placing them at the top of WHO’s risk criteria for COVID-19 related death. This is also true for about 40 percent of all home care clients.
Table 1: Characteristics of Nursing Home Residents and Home Care Clients in Canada, the United States, New Zealand and Finland22
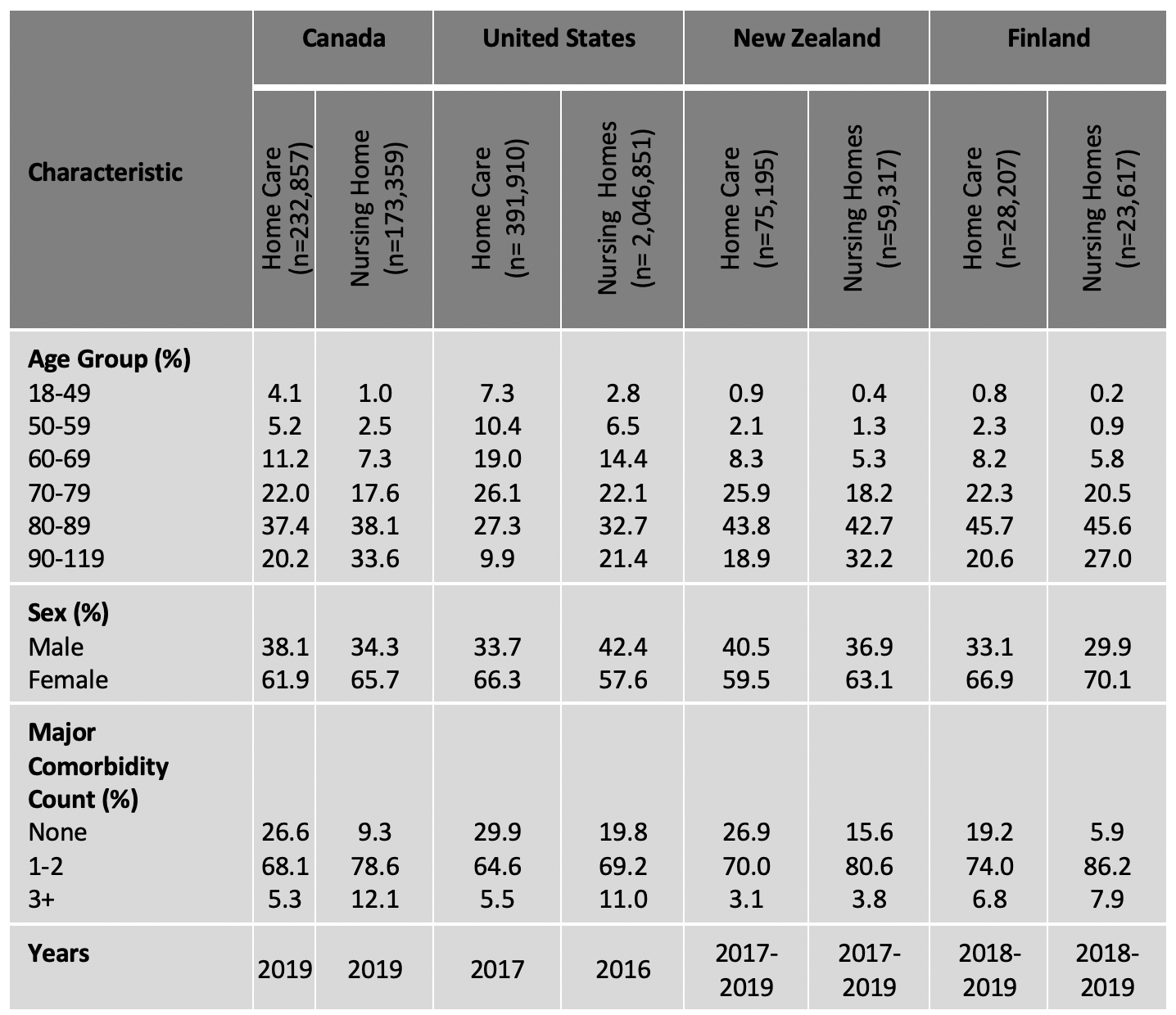
Despite serving similar populations, LTC facilities in these four countries had divergent experiences with the pandemic. Canadian and US nursing home death rates greatly exceeded predictions, but the rate was more moderate in Finland (146 deaths among 56,000 LTC residents). However, New Zealand’s nursing homes had only 14 deaths and 39 infected residents for the entire nation. Some of this was due to New Zealand’s stringent approach to containment of community spread, but there were also notable differences in the health system response to protecting nursing home populations.
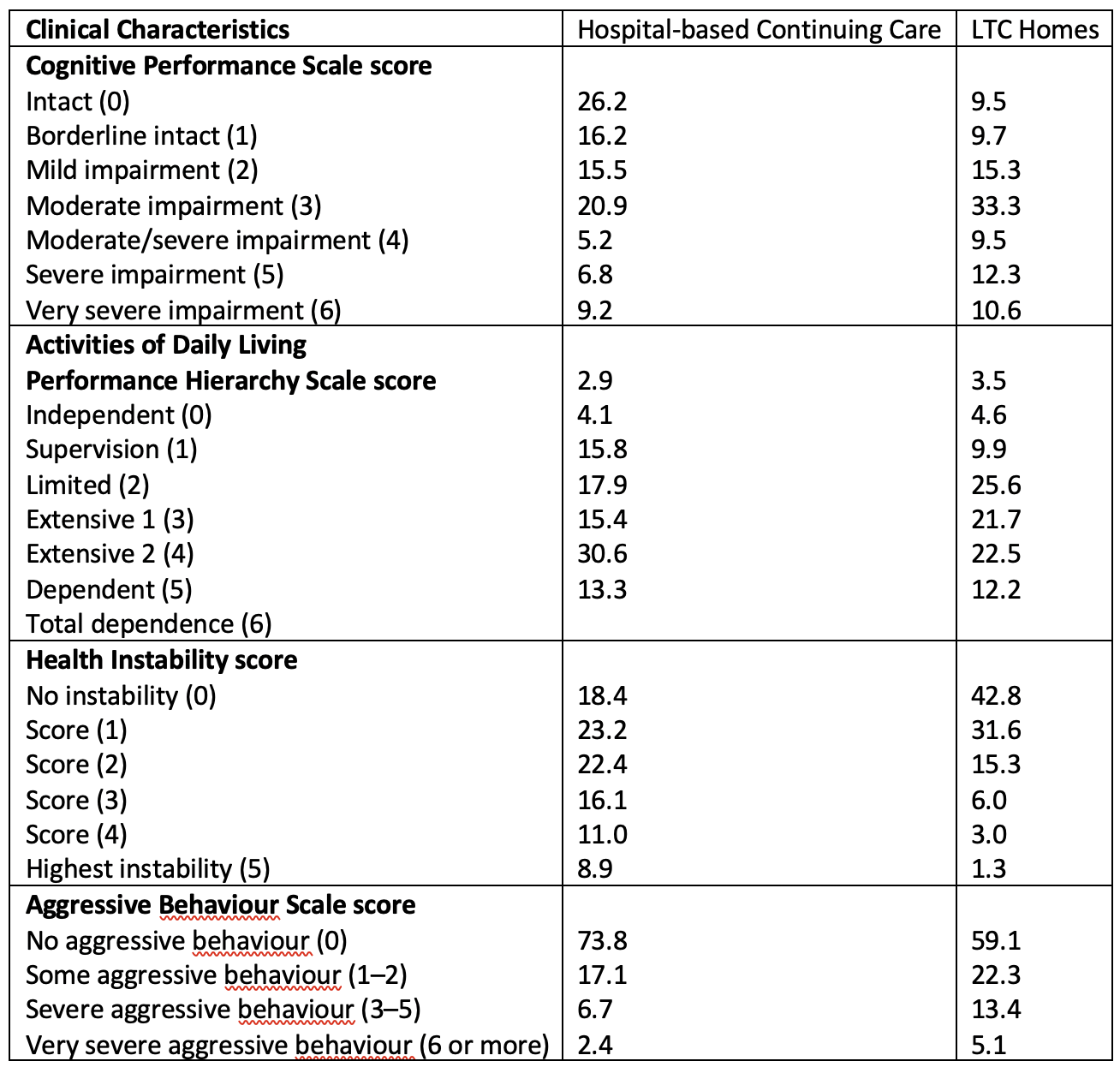
Table 2 compares the populations in Canadian nursing homes with hospital-based continuing care, using data from the Canadian Institute for Health Information’s (CIHI’s) Continuing Care Reporting System. Considering four dimensions of clinical need (cognitive impairment, physical disability, unstable health status and behavioural problems), there are distributional differences between the two care settings, but there are also substantial overlaps in the populations served. One-third of LTC residents have moderate to very severe cognitive impairment. More than half have extensive to total impairment in physical functioning, about one-quarter have substantial instability in health, and almost one-fifth have severe behavioural problems.
Table 2: Clinical Characteristics of Patients in Hospital-based Continuing Care and LTC Homes, Canada (2019)23
Despite the substantial care needs of LTC residents, these patients received much less clinical care than their counterparts in hospital-based continuing care. Table 3 shows that LTC residents received about half of the average nursing minutes of care per day and received 74 percent of that care from personal support workers (PSWs), compared to their counterparts in continuing care hospitals who received 90 percent of their care from registered nurses or registered practical nurses. Hospital-based patients received more than four times as much rehabilitation, compared with those in nursing homes. The majority of that care came from physical or occupational therapists, compared with only eight percent of the limited rehabilitation provided in LTC homes.
Table 3: Clinical Resources Available in Hospital-based Continuing Care and LTC Homes, Ontario, Canada (2007)24
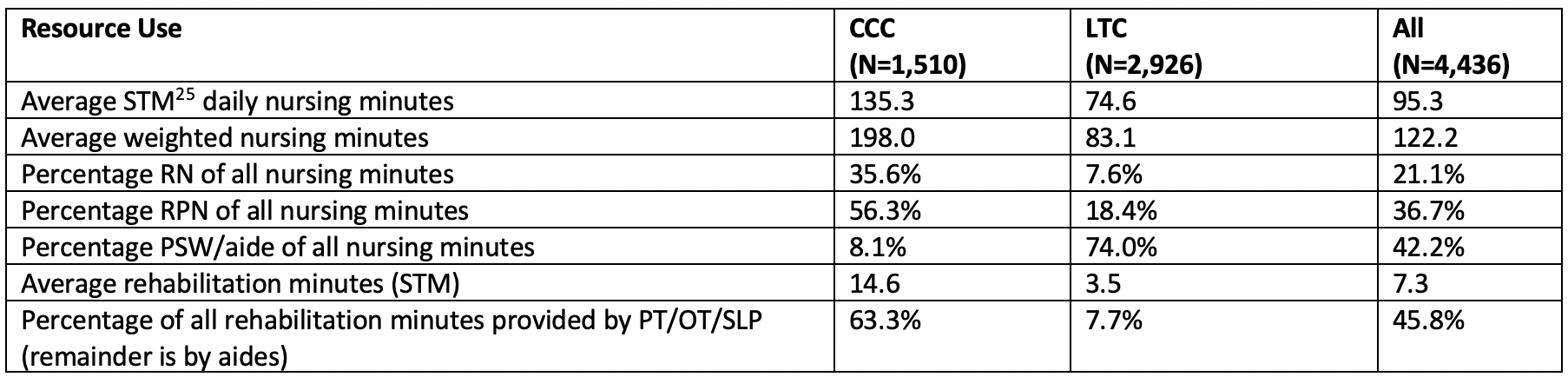
The service model of care in LTC homes is predominantly based on PSWs providing physical assistance, with threadbare support from registered health professionals. Hence, it comes as little surprise that many, but not all, of these homes were unprepared for the clinical threat posed by COVID-19. Most homes kept the coronavirus outside the facility. However, when the virus did enter, the infection often initially overwhelmed the staff’s capacity to contain its clinical impact.
Governments will need to make substantial financial commitments to adequately enhance clinical services in LTC. The challenge will be to ensure that additional funding is translated directly into additional hours of clinical care in a sector with mixed for-profit, charitable and government-run homes. Additional funding should apply to more direct care time, increased clinical expertise in geriatrics, better education, better care planning and ongoing review of performance against care expectations.
2) Collaboration to Improve Quality of Care and Quality of Life
A distinction is often made between LTC homes as places where people live and hospitals as places where people go for time-limited health care. Culture change initiatives in many LTC organizations emphasize transitioning away from a medical model of care to a more social model that is person-centred. Choice, respect, dignity, meaningful engagement, shared decision making and social relationships are central tenets of this new approach.
There is also a movement to transform physical environments from old institutional structures to physical spaces that have a more home-like feel and a greater sense of community engagement. This includes a move from congested multi-resident rooms to a greater proportion of single rooms.26 Redesigning homes for vulnerable older adults may result in more pleasant environments (for residents and outside visitors alike), with greater privacy for residents. This could in turn result in greater family and community engagement in the life of the facility. Nonetheless, the majority of the future populations living in these spaces will be affected by severe dementia, restricted mobility and numerous clinical complications. These will not be the preferred residential alternatives of independent older adults who want to interact socially with their neighbours.
Architectural designs that provide more private rooms have the added benefit of reducing the risk of spread of infectious disease, compared to older homes with up to four-person bedrooms. These architectural changes do not guarantee, however, that residents will not be inappropriately crowded into spaces intended for smaller numbers of individuals, as occurred with devastating consequences in one US veterans’ facility.27
The transition to an LTC culture that emphasizes quality of life need not, and should not, come at the expense of clinical quality of care. The expectation of being treated with humanity should not require forfeiture of excellent clinical care for the complex needs of frail older adults. Indeed, the Institute for Healthcare Improvement’s Triple Aim Initiative states that high-performing organizations are those that improve health, improve the experience of care and reduce the per capita costs of care simultaneously.28 This requires both the commitment and capacity to enact change by the administrative and clinical staff of the organization. It also depends on leadership from government, professional colleges, industry associations and advocacy groups to endorse expectations of quality improvement as central requirements for LTC. However, it is not always easy to foment change in isolation and with limited analytic capacity in individual organizations.
The Seniors Quality Leap Initiative (SQLI) is a promising model of how a community of practice can be established to drive positive change in quality of care and quality of life in LTC homes.29 SQLI is a network of 11 organizations serving more than 11,000 residents in 68 LTC homes in Canada and the United States. This group collaborates through virtual and in-person meetings to use evidence based on clinical quality of care indicators and quality of life metrics to establish common change initiatives, based on performance within the network and with national benchmarks in Canada and the United States. Partner agencies in the network include the CIHI, the Canadian Foundation for Healthcare Improvement, Accreditation Canada, research centres in Canada and the United States, LeadingAge, the New Brunswick Association of Nursing Homes and the interRAI research network. This collaborative has successfully improved pain management and appropriate use of anti-psychotic medications as its first two quality initiatives.30
With only modest support, such a model could scale up at the provincial, state or national levels. The key commitments are to use common performance measures, engage in knowledge exchange and collaboration to implement change strategies, share evidence on both successful and failed initiatives, understand how and when staffing and professional involvement makes a difference, continuously benchmark home-level data with national standards, and support full transparency within the network combined with de-identified external reporting. Rather than “blame and shame,” the emphasis is on joint pursuit of quality through bringing the “plan, do, study, act” cycle of change31 to life in LTC.
3) Enhancing the Evidence Base in LTC
Meaningful change is impossible without evidence. Canada, Belgium, Finland, New Zealand and the United States have implemented (or are about to implement) national assessment systems based on the interRAI standard.32 Use of these standardized assessment instruments in nursing homes support need identification, outcome measurement, resource allocation and performance measurement at the national level. This information can lead to greater understanding of the pandemic and the approaches that might result in better preparation for future threats to the lives and well-being of the elderly in LTC. One illustrative example is the CIHI’s Your Health System website, which provides publicly accessible reports at the home, chain, regional, provincial and national levels, with nine risk-adjusted outcome-based quality indicators for 1,287 nursing homes.33 Similar systems are in place or in development in other countries.34
Although Canada has had a sophisticated clinical evidence base in place for nursing homes for many years, the COVID-19 pandemic revealed some important information gaps that must be addressed to manage a national (or local) response to future pandemics.
First, it is not enough to simply have a great deal of data in a national data repository. The data must be current and must be ready for rapid mobilization. Canada has more than six million assessment records for nursing homes in a national reporting system, but the most recent data available were about six months out of date when the pandemic began. This has led to calls for establishment of a near-real-time reporting system that would provide decision makers with clinically relevant data about LTC home residents that is only days, rather than months, old.
Second, there is often limited expertise and few resources to maintain, analyze and apply such data to policy and practice. CIHI plays a substantial national role in this regard in Canada, but few countries have comparable organizations in place. Too often, there is a reliance on one-time analyses done by external contractors, instead of maintaining a regular analytic staff to address problems as they arise. Moreover, little attention is given to monitoring changes in health indicators that could be the “canary in the mine” for emerging problems.
Third, major gaps in public health information systems excluded nursing homes from routine reports about the COVID-19 pandemic. In Canada and the United Sates, the only time-sensitive sources of information about LTC deaths and infections have been the news media or university research groups that contacted local, state or provincial sources to fill in the gaps. In addition, these reports combined information about non-regulated retirement homes with regulated nursing homes serving a more resource-intensive population. Except in countries that had small numbers of deaths (New Zealand, for example), it has been almost impossible to obtain robust estimates about the precise numbers of persons affected by COVID-19 in LTC homes. LTC homes were “ground zero” for the pandemic in Canada and elsewhere, but they were not regarded as a priority for public health reporting.
Finally, many countries, including Canada, lack national standardized data on the characteristics of LTC homes. This includes basic information such as staffing levels, types of staff, facility age, room size and configuration, connections to hospitals (as part of a multicentre organization vs stand-alone, for example) and accreditation status. Some countries, such as the United States, have more of this type of information in place, but it may not cover both regulated and unregulated care settings.
4) Pandemic and Emergency Preparedness
Despite decades of warnings about imminent global pandemics, many countries were unprepared for the impact of COVID-19. In Canada, there was a singular focus on the hospital sector as the key setting to be bolstered. Elderly persons were discharged from hospitals to LTC homes to “make room for COVID-19 patients.” Earlier warnings from Italy about such practices went unheeded. Staff in LTC facilities and home care settings were told that in the absence of an outbreak they did not require personal protective equipment (PPE), which was in short supply nationally and being reserved for use in hospitals. Federal interim guidance on containment of COVID-19 in LTC was released more than three weeks after the pandemic was declared.
These experiences were not unique to Canada; however, some international counterpoints stand out. New Zealand has a comparable population receiving services in LTC homes, but that country has a long tradition of pervasive emergency preparedness owing to its vulnerability to earthquakes. New Zealand acted rapidly to close its international borders and contain community spread of the virus. While the District Health Boards’ emergency management teams focused on hospital and secondary care pandemic management, LTC homes took action to enact pre-established emergency protocols. An independent review of the COVID-19 clusters in LTC35 reported that providers enacted or adapted their up-to-date infection control documentation and procedures. The LTC homes provided refresher training on handwashing and use of PPE, and constrained access to homes; some acted even earlier than official advice. Hong Kong, like Canada, was greatly affected by the SARS pandemic of 2003. In response to that pandemic, Hong Kong required all homes to have a three-month supply of PPE on hand at all times. In South Africa, despite being a low-resource nation, its nursing homes in the Western Cape province were better prepared, with greater access to PPE, and widespread testing of staff and residents much sooner than in high-resource nations in North America and Europe. In Canada, the United States and other countries, PPE was virtually unavailable in LTC facilities, leaving staff and residents unprotected until the late stages of the first wave.
Failures in routine organizational practices added to the glaring gaps in emergency preparedness. Most governments paid inadequate attention to infection control in LTC homes before the pandemic, and staff were often poorly trained in how to prevent outbreaks and how to isolate or care for infected residents. Given the vulnerability of LTC home residents in ordinary times, standards for infection control must improve to avoid catastrophic outcomes in a pandemic.
5) Improving Quality of Work Life for LTC Staff
Staffing arrangements have likely been key contributors to adverse outcomes related to COVID-19 in LTC. Although little systematic evidence is available, poor wage rates, a lack of full-time work and sparse benefits have resulted in staff shortages in Canadian LTC homes. Jobs in this setting are less attractive and secure than in the food and hospitality industries. Reliance on part-time employment with low wages has also meant that staff work in multiple care homes (or other service sectors), which greatly increases risk of cross-contamination between homes.
In some homes, working conditions place great burdens on a small number of PSWs, resulting in high rates of injury and burnout. Inadequate staffing levels may result in rushed care, leading to increased physical and mental health complications in already frail residents. As the pandemic rose in severity, staff in many LTC homes became ill.36 COVID-19 being spread by asymptomatic carriers complicated matters, because simple temperature checks or quick, perfunctory screening could not prevent all cases of the virus entering the facility.37 Efforts to deal with substantial staff shortages in the midst of the pandemic may also have contributed to the spread of the virus.38
Despite very low rates of outbreaks, New Zealand’s LTC workers reported considerable stress related to the management of COVID-19 risk. Some felt the swab testing process for staff was thorough and well-managed, but others reported feelings of uncertainty, combined with pressure to decide between going to work or having contact with family. On the other hand, some managers and staff conveyed an increased level of camaraderie and pride at work. Staff turnover dropped during the four weeks of lockdown, as did sickness and absenteeism. LTC providers said they increased wellness initiatives for their staff, recognizing the effects of the pandemic on their workload and well-being.
Providing LTC home staff a living wage, adequate benefits, and stable employment arrangements are necessary, but insufficient, changes to ensure better quality of care. We must also reconsider the training provided to these staff and reimagine their roles as part of the clinical team. Examples include: training PSWs with an interprofessional educational approach, enhanced gerontological education, role modelling and mentoring situated directly in LTC;39 and the Netherlands’ three-year training program in elderly care medicine, which aims to enhance the skills of physicians to respond to the needs of frail older adults in community- and facility-based settings.40
Closing Remarks
What must we do to realize positive change as an outcome of this tragedy? First, action must be timely. Prolonged wrangling over bureaucratic or political minutiae cannot be allowed to hinder meaningful reform. This will require federal and provincial (or state) governments to act collaboratively instead of falling into traditional territorial traps. Second, changes must be decisive and profound. Half measures will not make a difference in a sector that has languished at the periphery of the health care system. Third, change must be informed by evidence. There must be a clear commitment to enhancing available data systems to fill key information gaps. We must mobilize high-quality data to engage all stakeholders in an open, transparent dialogue about the nature of our response. Such data systems will help to identify what challenges require action and will also provide evidence about the adequacy of our response over time. We owe it to the victims of the LTC pandemic to commit to meaningful, permanent change so these events remain in our past rather than posing a threat to our future.
About the authors
John P. Hirdes, Professor, School of Public Health and Health Systems, University of Waterloo (Canada); Anja Declercq, Professor, LUCAS, Centre for Care Research and Consultancy and CESO, Center for Sociological Research, KULeuven (Belgium); Harriet Finne-Soveri, Visiting Professor, National Institute for Health and Welfare, Helsinki (Finland); Brant E. Fries, Professor Emeritus, Department of Health Management and Policy, University of Michigan (USA); Leon Geffen, Director, Samson Institute for Ageing Research, Cape Town (South Africa); George Heckman, Schlegel Research Chair in Geriatric Medicine, Schlegel Research Institute for Aging, University of Waterloo (Canada); Terry Lum, Henry G. Leong Professor Department of Social Work and Social Administration, University of Hong Kong (Hong Kong); Brigette Meehan, MNZSTA Adjunct Professor, Massey University and Principal Advisor, interRAI Services, TAS, Wellington (New Zealand); Nigel Millar, FRACMA Geriatrician and CMO, Southern District Health Board, Dunedin (New Zealand); John N. Morris, Director Emeritus of the Marcus Institute for Aging Research, Hebrew Senior Life, Boston (USA)